These answer explanations are and always will be free. However, given multiple email requests, I will post my Venmo (@Adam-Zakaria-SLO) if you want to send a few dollars to show your support for the website.
I also offer reasonably priced Study Guides and Personalized Study schedules, so please reach out using the Tutoring menu option or Study Guides and Personalized Study schedules menu option listed above if you would like personalized support.
Furthermore, I offer personal statement and application review services for residency applicants, so please reach out using the “Residency Advising and Application Preparation” menu option above if interested.
Lastly, please check out my Youtube channel (https://www.youtube.com/channel/UCT1Ukl4pm5QK9iw6h4MB_Hw/playlists) and the “Biostatistics Curriculum” option above for free videos and practice questions reviewing all the essential biostatistics topics covered on NBME exams. Good luck with your exams!
1) A 22-year-old woman comes to the physician because she has had a black spot that occludes her vision in her right eye…
Cranial nerve 2
- Young woman presents with unilateral eye pain associated with a central scotoma, most concerning for multiple sclerosis complicated by optic neuritis (which is due to inflammation of the optic nerve (CN 2))
- Key idea: 2 eye conditions that are quite specific for multiple sclerosis include:
- Optic neuritis: Unilateral eye pain and visual problems
- Internuclear ophthalmoplegia: One eye cannot fully adduct on lateral eye movements
- Cerebellar lesion –> Ataxia (wide-based gait, impaired finger-nose testing)
- CN 3 –> “Down and out” eye +/- blown pupil (loss of parasympathetic tone) +/- ptosis
- CN 4 –> Trouble walking down stairs or reading (impaired lateral eye movements when looking down)
- CN 6 –> Unilateral issues with eye abduction
- MLF –> Internuclear ophthalmoplegia
- NM Junction –> Myasthenia gravis, Lambert-Eaton, botulism
2) A 47-year-old woman is brought to the emergency department 1 hour after the onset of a severe headache that began…
Posterior communicating
- Middle aged woman presents with “worst headache of her life” while exercising with exam notable for blown right pupil + meningismus most concerning for subarachnoid hemorrhage in setting of ruptured posterior communicating artery aneurysm
- Key idea: Aneurysms of the posterior communicating arteries commonly compress cranial nerve 3 and therefore lead to loss of parasympathetic tone to the eye, leading to mydriasis
- Key idea: Parasympathetic fibers run in Periphery of CN3 whereas Motor fibers run in the Middle, which is why compression of CN3 typically first leads to loss of parasympathetic function before causing “down and out” eye
- Key idea: Meningismus (pain with neck movements) can be seen in both meningitis (due to inflammation/infection of meninges) AND subarachnoid hemorrhage (due to blood accumulation in subarachnoid space irritating meninges)

3) An 80-year-old man briefly loses consciousness and falls to the floor in a grocery store. He awakens within 1 minute and feels…
Carotid sinus hypersensitivity
- Elderly man with recurrent loss of consciousness precipitated by bradycardia in the setting of head turning, most consistent with carotid sinus sensitivity
- Turning of head –> Increased pressure on carotid sinuses –> Increased baroreceptor response –> Increase parasympathetic tone to heart –> Decreased heart rate and contractility
- Note: The above mechanism is leveraged when we perform carotid massage in the setting of stable narrow complex tachycardias
- Key idea: In setting of loss of consciousness, first step is to determine seizure vs syncope, with presence of post-ictal state (suggestive of seizure) being the most reliable feature, followed by lateral tongue biting (again suggestive of seizure) [Note: urinary incontinence and shaking can be seen IN EITHER seizure or syncope]
4) A 37-year-old man comes to the physician because of a 6-month history of difficulty walking and a tremor of the right…
Discontinuing fluphenazine
- Young man with schizophrenia on a high-potency antipsychotic presents with resting tremor + slow movements (akinesia) + shuffling gait most concerning for the extrapyramidal symptom of Parkinsonism –> Manage by discontinuing the anti-dopaminergic medication
- Key idea: Psychosis is associated with increased dopamine activity whereas Parkinson’s disease is associated with decreased dopamine activity, which is why treatments for psychosis (which decrease dopamine levels) can lead to Parkinsonism and treatment for Parkinson’s disease (which increase dopamine levels) can lead to psychosis
- Key idea: High-potency antipsychotics have the highest risk of extrapyramidal side effects, with the common examples being haloperidol, fluphenazine, and trifluoperazine; another medication associated with extrapyramidal side effects is the promotility agent metoclopramide given it also is an anti-dopaminergic agent
- Extrapyramidal symptoms:
- Acute dystonia –> Forced flexion of neck and eyes, treat with diphenhydramine
- Akathisia –> Internal feeling of restlessness, treat with benzo or beta-blocker
- Parkinsonism –> TRAPS symptoms (resting Tremor, Rigidity, Akinesia, Postural instability, Shuffling gait), treat with benztropine
- Tardive dyskinesia –> Uncontrolled motions of face and mouth, discontinue antipsychotic and start valbenazine
5) A previously healthy 42-year-old man comes to the physician because of a 6-week history of intermittent pain…
Cervical nerve root compression
- Young man with pain/tingling of right upper extremity (involving thumb) worse with Valsalva with decreased right biceps reflex most concerning for compression of C6 nerve root
- Valsalva (coughing, sneezing, bearing down) –> Increased CSF pressure –> Increased compression of nerve roots trying to exit spinal cord (clue that we are dealing with nerve root compression > peripheral nerve pathology)
- Key idea: Remember that C6 provides sensation to the thumb because if you hold your thumb up with your left hand it looks like a 6
- Key idea: If patient had compression of the cervical spine, you would expect UMN symptoms in the lower extremities (increased reflexes, positive Babinski, etc.)
6) A 62-year-old man with amyotrophic lateral sclerosis comes to the physician because of a 1-month history…
Diaphragmatic paralysis
- Middle-aged man with ALS presents with progressive shortness of breath worse when lying flat with paradoxical breathing (abdomen collapsing inwards on inspiration) most concerning for diaphragmatic weakness
- Key idea: Patients with ALS commonly die as a result of respiratory arrest in the setting of diaphragmatic weakness
- Key idea: When patient is lying flat, they cannot be assisted by gravity in taking a deep breathe and therefore have worsening shortness of breathe
7) A 6-year-old girl is brought to the physician because of a 1-week history of progressive weakness and numbness of the legs…
Metastatic spread of the cancer through cerebrospinal fluid pathways
- Young girl with history of medulloblastoma presents with weakness/numbness of legs + urinary incontinence + “saddle anesthesia” + decreased lower extremity reflexes most concerning for “drop metastases” leading to cauda equina syndrome
- Key idea: Medulloblastoma classically leads to “drop metastases”, which is metastatic spread of the cancer through the CSF to the spinal cord
- Key idea: The cauda equina represents spinal nerve roots leaving from the conus medullaris (tip of the spinal cord), and therefore compression of the cauda equina leads to LOSS of lower extremity reflexes (in contrast to UMN symptoms seen with compression of spinal cord or conus medullaris)
8) A 45-year-old woman is brought to the emergency department 30 minutes after a generalized tonic-clonic seizure…
Nitroprusside
- Middle-aged woman presents with headache + seizure and is found to have BP > 180/120 with papilledema on fundoscopic exam (blurred optic disc margins), most consistent with hypertensive encephalopathy –> Treat with strong anti-hypertensive, with common options being nitroprusside, labetalol, nicardipine, clevidipine and fenoldopam
- Hypertensive urgency = Severe hypertension (>180/120) without acute end-organ damage
- Hypertensive encephalopathy = Severe hypertension + cerebral edema and neurologic signs/symptoms
- Malignant hypertension = Severe hypertension + retinal hemorrhages, retinal exudates and/or papilledema
9) A 62-year-old woman comes to the physician because of a 6-week history of stiffness and pain of her neck, shoulders and…
Polymyalgia rheumatica
- Middle-aged woman presents with proximal pain/stiffness WITHOUT true weakness on exam and is found to have a significantly elevated ESR, consistent with polymyalgia rheumatica
- Key idea: Although on UWorld polymyalgia rheumatica is often grouped with other myopathies (statin-induced, myositis, etc.), it leads to stiffness but NOT true weakness (AKA decreased strength on exam)
- Key idea: Polymyalgia rheumatica is associated with giant cell arteritis (unilateral headache + jaw claudication + visual symptoms), both of which are treated with corticosteroids
10) A 62-year-old man is brought to the emergency department because of a 1-week history of urinary hesitancy, leg weakness…
Dexamethasone
- Middle-aged man presents with subacute urinary hesitancy and lower extremity symptoms and is found to have tenderness over the midthoracic spine with UMN weakness in the legs and loss of sensation bilaterally below the costal margin, concerning for compression of the thoracic spinal cord –> Next best step is to start steroids (to limit inflammation/compression) and get an MRI to confirm
- Key idea: Vertebral point tenderness consistent with fracture, malignancy and osteomyelitis/epidural abscess, but paraspinal muscle tenderness most consistent with MSK-related back pain
- Mannitol –> Useful in setting of cerebral edema (causes blood to be hypertonic and therefore draw fluid out of the brain)
11) A 42-year-old man comes to the physician with his wife because of a 6-month history of increasing clumsiness and…
Atrophy of the caudate nucleus on brain imaging
- ~40 year old man presents with chronic progressive irritability and jerky, involuntary movements of his limbs concerning for Huntington disease (due to caudate nucleus atrophy)
- Key idea: Huntington’s disease typically presents around 40 years of age with chorea + cognitive changes + psychiatric disease (anxiety, depression, irritability)
- Key idea: Huntington’s disease classically demonstrates anticipation, such that if patients inherit the disease from their father they tend to have more trinucleotide repeats and therefore have an earlier age of onset of the disease
- Decreased serum methylmalonic acid concentration –> B12 deficiency (patient too young and doesn’t have risk factors)
- Dilated ventricles –> Hydrocephalus or schizophrenia
- Increased oligoclonal bands in CSF –> Multiple sclerosis
12) A 42-year-old woman comes to the physician because of a 4-day history of progressive weakness and numbness in her legs…
Aquaporin-4 autoantibodies in the cerebrospinal fluid
- Young woman presents with multiple sclerosis-like picture (neurologic symptoms disseminated in time/space with imaging demonstrating periventricular white matter lesions), but has bilateral optic neuritis + no oligoclonal bands in CSF + significant spinal cord disease and therefore is most compatible with neuromyelitis optica syndrome (which is diagnosed by presence of aquaporin-4 autoantibodies)
- Key idea: Main features that distinguish neuromyelitis optica syndrome from MS include:
- Lack of oligoclonal bands in CSF
- Large segments of myelitis
- Severe optic neuritis
- Area postrema syndrome (intractable vomiting and/or hiccups)
13) A 30-year-old construction worker comes to the physician because of constant midlower back pain…
Restriction of heavy lifting until the pain resolves and instruction in proper body mechanics
- Young man with active job presents with subacute back pain with negative straight leg test (given symptoms don’t radiate down leg), and therefore should be treated conservatively as MSK lower back pain with 4-6 weeks of NSAIDs and maintained activity as tolerated
- Key idea: These patients SHOULD NOT spend significant time on bed rest given it can delay recovery
14) A 56-year-old woman is brought to the emergency department 20 minutes after a simple partial seizure. A CT scan…
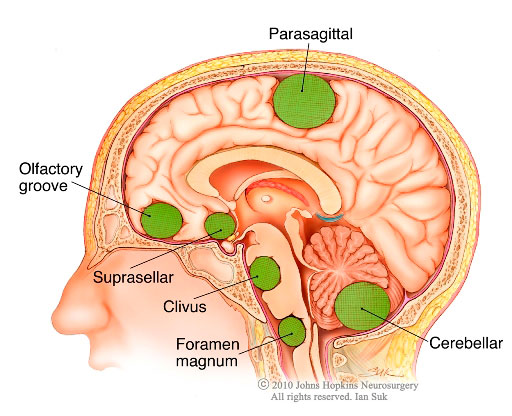
Meningioma
- Middle-aged woman presents following a seizure and is found to have a uniformly enhanced parasagittal mass in the frontal lobe most concerning for a meningioma
- Key idea: Meningiomas (as the name implies) tends to occur on the outer surface of the brain (rather than within the parenchyma) given they are derived from the meninges
- Schwannoma –> Classically present in brainstem and pontomedullary junction (thereby compressing CN 5, 7 and/or 8)
- Glioblastoma multiforme –> Advanced brain cancer that often involves both hemispheres in advanced stage
- Ependymoma –> Intra or peri-ventricular tumor (given it’s derived from cells lining ventricles)
15) A 14-month-old infant is brought to the physician because of four episodes of loss of consciousness over the past…
Breath-holding episode
- Infant presents with recurrent episodes of cyanosis and loss of consciousness associated with breath-holding while crying with spontaneous return to normal behavior most consistent with breath-holding episodes
- Key idea: Breath-holding spells commonly seen in children 6 months to 2 years of age, with the two primary types being:
- Cyanotic: Crying –> breath holding –> cyanosis and loss of consciousness
- Pallid: Minor trauma/injury –> breath holding –> pallor + diaphoresis + loss of consciousness
16) A 52-year-old man is brought to the emergency department from work 30 minutes after the sudden onset of…
Conversion disorder
- Middle-aged man who had a stressful event at work presents with reported blindness but has a completely normal exam (including with reaction to movement towards his face) with indifference, most consistent with conversion disorder
- Key idea: As the name implies, conversion disorder is thought to represent subconscious conversion of psychological/emotional distress into physical neurologic symptoms
- Key idea: Patients with conversion disorder classically demonstrate “la belle indifference”, meaning that they don’t have any stress/concern/worry about their symptoms
- Malingering –> Patient consciously making up symptoms for obvious gain, patients would often be trying to overemphasize their symptoms rather than seem indifferent towards them
17) A 35-year-old woman comes to the physician because of a 14-day history of progressively severe headache…
Intravenous amphotericin B
- Middle aged woman on immunosuppression presents with subacute headaches, fevers and meningismus with lumbar puncture demonstrating monocytic leukocytosis with low glucose, most concerning for mycobacterial versus fungal meningitis (specifically cryptococcal meningitis) –> Treat with amphotericin B (antifungal)
- Key idea: Cryptococcal meningitis seen in immunocompromised patients and classically leads to signs of increased intracranial pressure (papilledema, CN6 palsy, etc.)
- Key idea: Normal CSF glucose should be ~2/3 of blood glucose, so given a normal blood glucose is around 100 a normal CSF glucose is around 60-70
- CSF findings of infectious pathogens:
- Bacterial: Neutrophilic predominance, really high WBCs, low glucose
- Fungal/Mycobacterial: Lymphocytic/Monocytic predominance, low glucose
- Viral: Lymphocytic predominance, normal glucose
18) A 57-year-old woman comes to the physician because of a 2-day history of dribbling fluid from her mouth every time…
Prednisone therapy
- Middle-aged woman presents with acute weakness of the entire left side of her face, concerning for Bell’s palsy (CN7 palsy) –> Treatment is corticosteroids +/- acyclovir
- Key idea: To distinguish between UMN cause of facial weakness (e.g., stroke) and LMN cause of facial weakness (e.g., Bell’s palsy), look for forehead involvement which is indicative of a LMN lesion given the forehead receives input from both UMN but only the ipsilateral LMN
- Common causes of Bell’s palsy:
- HSV (most common!)
- VZV (leads to Ramsay-Hunt syndrome with painful vesicles within ipsilateral ear)
- Sarcoidosis
- Salivary tumors
- Lyme disease (BILATERAL Bell’s palsy)

19) A 62-year-old woman is brought to the emergency department after an episode of flaccid paralysis and numbness…
Cerebral embolus
- Middle-aged woman presents following an episode of left-sided weakness, sensory changes and vision loss that resolved on its own with a normal head CT, most consistent with a transient ischemic attack –> Often represents sequelae of embolic phenomenon
- Common sources of embolic stroke:
- Atrial fibrillation (stasis in LA leads to clot formation in left atrial appendage)
- LV aneurysm (recent MI –> lack of LV wall movement –> blood stasis –> clot formation adjacent to damaged LV wall)
- Carotid atherosclerosis (pieces of plaque flick up into brain)
- Endocarditis
- Key idea: In keeping in mind the common sources of emboli, standard work-up following a stroke with unknown source includes:
- Carotid doppler (looking for carotid atherosclerosis)
- EKG followed by Holter monitor (looking for atrial fibrillation)
- Echo (looking for endocarditis and/or LV aneurysm)
- Lacunar infarct –> Patient with poorly controlled hypertension who presents with pure motor or pure sensory stroke
- Rupture of cerebral artery aneurysm –> Subarachnoid hemorrhage (“worst headache of my life” + meningismus)
20) A 32-year-old man comes to the physician because of a 6-month history of deep aching neck and shoulder pain…
Syringomyelia
- Young man with history of whiplash injury presents with chronic progressive weakness of the hand associated with decreased pain sensation over the arms and shoulders in a “cape-like” distribution, most consistent with syringomyelia
- Key idea: Syringomyelia commonly develops following trauma or in association with Arnold-Chiari malformation type 1 (cerebellar herniation)
- Key idea: Syringomyelia is a cyst in the middle of the spinal cord, and therefore the initial symptoms typically involve loss of pain/temperature sensation given the spinothalamic tract crosses within the spinal cord itself –> later on it can expand to involve the anterior corticospinal tract and thereby lead to upper extremity weakness
- ALS –> Intrinsic hand weakness + esophageal/pharyngeal weakness + mixed UMN and LMN weakness
- Subacute combined degeneration (B12 deficiency) –> Damage to Spinocerebellar tract (ataxia), Corticospinal tract (motor weakness) and Dorsal column tract (sensory tract)

21) An 82-year-old woman is brought to the physician because of a 6-month history of neck pain radiating to her left…
Cervical spondylotic myelopathy
- Elderly woman with history of osteoarthritis presents with chronic progressive neck pain + weakness/atrophy of the hands/forearms with decreased upper extremity reflexes (indicative of LMN weakness) + UMN signs of the lower extremities (increased reflexes, Babinski) most consistent with cervical spine compression due to cervical spine osteoarthritis
- Key idea: When a patient has LMN weakness at one spinal level and then UMN weakness everywhere below, that is often consistent with spinal cord compression at the level of the LMN weakness
22) A 67-year-old woman is brought to the emergency department 1 hour after the sudden onset of right facial weakness…
Pons
- Elderly woman with history of hypertension and 35 pack-year smoking use presents with sudden onset right facial weakness (including forehead) + decreased hearing and tinnitus on right + right-sided ataxia most consistent with a lateral pontine stroke
- HIGH-YIELD: Rule of 4’s below can help you develop system for localizing brainstem lesions (recommend Boards & Beyond video)
- Key idea:
- Medial midbrain –> CN3 and CN4 defects
- Medial pons –> Locked-in syndrome
- Lateral pons –> CN7 defect is specific finding
- Medial medulla –> CN12 defect is specific finding
- Lateral medulla –> CN 10/11 defect is specific finding

23) A 47-year-old man is brought to the emergency department by police after he was found in a state of confusion outside a convenience…
Delirium tremens
- Middle-aged man with significant alcohol use history is found to have anxiety/agitation + altered mental status + sympathetic hyperactivity (tachycardia, hypertension, diaphoresis) concerning for delirium tremens
- Key idea: Chronic alcohol use leads to downregulation of inhibitor GABA receptors and upregulation of stimulatory NMDA (glutamate) receptors, such that patients can become hyperactivity if they stop using alcohol
- Manifestations and timing of alcohol withdrawal
- 0-24 hours –> Mild withdrawal
- 12-48 hours –> Seizures
- 12-48 hours –> Hallucinations (visual, auditory, tactile)
- 48-96 hours –> Delirium tremens (confusion, agitation, sympathetic hyperactivity)
24) A 67-year-old woman is brought to the physician because of progressive imbalance and memory difficulties over…
Progressive supranuclear palsy
- Elderly woman with chronic history of Parkinson’s-like symptom (rigidity, shuffling gait, signs of chronic neurodegeneration on head imaging) who also has many falls + vertical gaze palsy most consistent with one of the Parkinson-plus syndromes of Progressive supranuclear palsy
- Signs/symptoms of Parkinson’s disease can be remembered by mnemonic TRAPS:
- Tremor (resting, can be asymmetric)
- Rigidity
- Akinesia (slow movements)
- Postural instability (can’t catch themselves if they fall)
- Shuffling gait
- The main Parkinson’s-plus syndromes to recognize include:
- Progressive supranuclear palsy: Parkinson’s + falls + vertical gaze palsy
- Multiple system atrophy: Parkinson’s + autonomic dysfunction (orthostatic hypotension, urinary/bowel incontinence, problems with thermoregulation, dry mouth/eyes, erectile dysfunction, etc.)
- Wernicke encephalopathy –> Patient at risk for nutritional deficiency (alcoholism, eating disorder, etc.) presenting with triad of confusion + ataxia + ophthalmoplegia
25) A 62-year-old man comes to the physician because of a 4-month history of progressive difficulty climbing stairs…
Smoking cessation
- Middle-aged man with 60 pack-year smoking history with a known lung nodule presents with chronic progressive proximal muscle weakness + autonomic dysfunction (dry mouth) + decreased reflexes + increased amplitude motor responses with repeated stimulation (“improves with use”) most consistent with small cell lung cancer complicated by Lambert-Eaton syndrome –> Smoking would have prevented development of small cell lung cancer
- The three major neuromuscular junction pathologies include:
- Myasthenia gravis (autoantibodies against post-synaptic acetylcholine receptors): Proximal muscle and oculobulbar weakness that worsens with repeated use in a patient with a thymoma
- Lambert-Eaton syndrome (autoantibodies against pre-synaptic calcium channels): Proximal muscle weakness + autonomic dysfunction + loss of reflexes in a patient with small cell lung cancer
- Botulism (toxin preventing release of Acetylcholine into synaptic cleft): Descending weakness with oculobulbar weakness in a patient who ate canned food or a newborn who ate honey
26) After falling from a horse during steeplechase, a 42-year-old man has immediate paralysis in all four extremities and has…
Intravenous methylprednisolone therapy
- Young man who presents with quadriplegia and loss of sensation below the neck after falling off a horse, most concerning for cervical spinal cord injury/compression (as confirmed by spinal imaging) –> Best first step is IV corticosteroids to decrease spinal cord inflammation/edema
27) An 87-year-old man comes to the physician because of headaches over the past 6 weeks; they fluctuate…
Subdural hematoma
- Elderly man on aspirin presents with chronic intermittent headaches + asymmetric upper motor neuron signs in the upper and lower extremities (pronator drift, increased reflexes, Babinski sign) most concerning for Subdural hematoma
- Key idea: Elderly patients are very prone to having subdural hematomas because people’s brains atrophy as they get older –> bridging veins travel longer distance unprotected and are at high risk of damage in setting of acceleration-deceleration injury (i.e., fall)
- Key idea: Presence of upper motor neuron signs tells you there is pathology in the brain, brainstem or spinal cord
- Craniopharyngioma –> Pediatric patient with bitemporal hemianopsia +/- hypopituitarism
- Hypertensive encephalopathy –> BP > 180/120 + confusion + papilledema
- Major depressive disorder –> Would not have unilateral neurologic findings, SIGECAPS
- Temporal arteritis –> Elderly patient with unilateral headache associated with temporal tenderness + jaw claudication, associated with polymyalgia rheumatica (stiffness/pain of shoulders and hips)
28) A previously healthy 82-year-old man is brought to the emergency department because of a 3-hour history of…
Dysrhythmia
- Elderly man presents with acute onset of Wernicke aphasia (able to speak, but words do not make sense and they do not understand other’s speech) and right pronator drift found to have atrial fibrillation on ECG, most consistent with ischemic stroke to the left MCA due to an embolus from the left atrial appendage in the setting of atrial fibrillation
- Key idea: Damage to left temporal lobe leads to Wernicke aphasia (expressive aphasia, does not understand speech) whereas damage to left frontal lobe leads to Broca’s aphasia (non-expressive aphasia, understands speech)
- Common sources of embolic stroke:
- Atrial fibrillation (stasis in LA leads to clot formation in left atrial appendage)
- LV aneurysm (recent MI –> lack of LV wall movement –> blood stasis –> clot formation adjacent to damaged LV wall)
- Carotid atherosclerosis (pieces of plaque flick up into brain)
- Endocarditis
- Key idea: In keeping in mind the common sources of emboli, standard work-up following a stroke with unknown source includes:
- Carotid doppler (looking for carotid atherosclerosis)
- EKG followed by Holter monitor (looking for atrial fibrillation)
- Echo (looking for endocarditis and/or LV aneurysm)
29) A 35-year-old woman has had constant burning pain in her right hand since closing her hand in a car door…
Abnormal sympathetic neural response
- Young woman with history of trauma to the right hand who presents 1 year later with chronic burning pain and excessive tenderness, most concerning for complex regional pain syndrome (due to abnormal sympathetic neural responses)
- Key idea: Classic presentation involves trauma/surgery to an area of the body followed by:
- Severe pain (often burning/stinging)
- Edema
- Abnormal sweating
- Altered skin temperature
- Skin, hair or nail changes to the area
- Increased intracarpal canal pressure –> Wrist pain + sensory loss to lateral palm (including thumb); often worse at night
30) A 25-year-old woman has had generalized weakness for 2 days. On questioning, she reports numerous hospital admissions…
Acute intermittent porphyria
- Young woman with history of recurrent abdominal pain presents with acute onset weakness, areflexia and lower extremity sensory loss, concerning for acute intermittent porphyria
- Acute intermittent porphyria classically leads to 5 P’s
- Painful abdomen (intermittent abdominal pain WITHOUT tenderness [neuropathic])
- Port-wine (reddish) urine
- Polyneuropathy (sensory changes, weakness, loss of reflexes)
- Psychiatric disease (anxiety, depression, hallucinations, etc.)
- Precipitated by P450 inducers (alcohol, barbiturates, rifampin, etc.)
- Leprosy –> Anesthetic macular lesions + thickened nerves
- Guillain-Barre –> Ascending lower extremity weakness, sensory changes and loss of reflexes that develop over weeks
31) A 67-year-old man with a 30-year history of alcoholism is brought to the emergency department 1 hour after he was found…
Intravenous vitamin B1 (thiamine) therapy
- Elderly man with chronic history of alcoholism is found confused and malnourished with exam notable for disconjugate gaze, most concerning for Wernicke encephalopathy (Vitamin B1 deficiency) –> Give THIAMINE BEFORE GLUCOSE
- Key idea: Wernicke encephalopathy seen in patients with risk factors for malnourishment (alcoholism, eating disorders, etc.) and presents with triad of confusion, ataxia and ophthalmoplegia
- Key idea: Commonly tested concept is that in patients who are found down with suspected alcoholism or unknown history you should give thiamine before glucose because if you give glucose first it may drive the little available thiamine into the cell and precipitate Wernicke encephalopathy
- Note: May be a medical myth (but still gets tested) – https://pubmed-ncbi-nlm-nih-gov.ucsf.idm.oclc.org/22104258/
32) A 57-year-old woman comes to the physician because of daily headaches for 8 months. The headaches…
Temporomandibular joint syndrome
- Middle-aged woman with recent increase in stress presents with daily headaches in her temple exacerbated by movements of the jaw with tenderness at the zygomatic arch and a normal ESR, most consistent with temporomandibular joint syndrome
- Temporal arteritis –> Elderly patient with temporal headaches + jaw claudication + elevated inflammatory markers +/- polymyalgia rheumatica (pain/stiffness in proximal joints)
- Key idea: Initiate corticosteroids before getting temporal artery biopsy given risk of blindness!
- Trigeminal neuralgia –> Shooting pain in the face that lasts for seconds-minutes and is often exacerbated by chewing, talking and/or touching certain parts of the face
33) A 72-year-old man with a history of atrial fibrillation comes to the emergency department 2 hours after the sudden onset…
Left posterior cerebral
- Elderly man with atrial fibrillation presents with sudden onset loss of visual acuity in his right visual field, most consistent with damage to the ocular tract behind the optic chiasm, including potentially the left occipital lobe (given occlusion of the left posterior cerebral)
- Homonymous hemianopsia (AKA loss of vision on same side in both eyes) –> Damage to optic tract behind the optic chiasm (fibers haven’t crossed over)
- Bitemporal hemianopsia (AKA loss of outer aspect of visual field) –> Damage at the optic chiasm
- Monocular vision loss (AKA loss of vision from one eye) –> Damage to optic tract in front of the optic chiasm (fibers have already crossed over)
- Key idea: The left occipital cortex is responsible for the right visual fields, and vice versa
- Common sources of embolic stroke:
- Atrial fibrillation (stasis in LA leads to clot formation in left atrial appendage)
- LV aneurysm (recent MI –> lack of LV wall movement –> blood stasis –> clot formation adjacent to damaged LV wall)
- Carotid atherosclerosis (pieces of plaque flick up into brain)
- Endocarditis

34) A 25-year-old woman comes to the physician because of a 1-year history of depressed mood and episodes of daytime…
Narcolepsy
- Young woman with persistent daytime sleepiness requiring daily naps, with these naps being associated with hypnagogic and hypnopompic hallucinations, most consistent with narcolepsy
- Key idea: Narcolepsy defined by recurrent lapses into sleep/naps along with:
- Cataplexy (falling to ground when laughing, crying, etc.)
- Low CSF levels of hypocretin-1
- Shortened REM sleep latency on polysomnography
- Note: Can also be associated with hypnagogic and hypnopompic hallucinations (hallucinations when falling asleep and waking up), but not formal criteria
- Nightmare disorder –> Recurrent episodes or significant stress from recurrent nightmares while sleeping that patient remembers upon waking
35) A 7-year-old girl is brought to the physician because of progressive sleepiness, ataxia, and double vision over…
Carbamazepine-erythromycin interaction
- Young girl chronically on carbamazepine for seizure disorder who has been on erythromycin for the past week presents with several days of ataxia and double vision, most concerning for carbamazepine toxicity in the setting of erythromycin-driven inhibition of P450 enzymes
- Key idea: Carbamazepine is an anti-epileptic that helps to “calm the mind”, so if a patient takes too much of it they will be “too calm) –> Altered mental status, ataxia, drowsiness, etc.
36) A 77-year-old man is brought to the physician by his daughter because he has become increasingly forgetful during the…
Lumbar puncture
- Elderly man presents with chronic progressive memory loss and is found to have ataxia, intermittent episodes of urinary incontinence/constipation and a brain MRI showing slightly enlarged ventricles despite minimal cortical atrophy, concerning for possible normal pressure hydrocephalus –> Next best step is lumbar puncture to measure CSF pressure (and potentially help patient feel better!)
- Normal pressure hydrocephalus –> Wet, Wacky, Wobbly = Urinary incontinence, Confusion/Memory problems, Ataxia
37) A 72-year-old man comes to the physician because of a 1-week history of imbalance and leg weakness and a…
Epidural spinal cord compression
- Elderly man with 50 pack-year smoking history and chronic weight loss/cachexia presents with acute leg weakness and bladder issues and is found to have lower extremity weakness with UMN signs (hyperactive reflexes, Babinski sign) and sensory loss between the umbilicus, most consistent with spinal cord compression at the T10 level most likely in setting of metastatic cancer
- Key idea: In setting of acute spinal cord compression, IV steroids are often indicated to reduce spinal cord inflammation/edema
- Note: Transverse myelitis could also lead to pathology involving the spinal cord, but would be more expected in a young patient (given increased risk of autoimmune disease) and this patient clearly has a story consistent with possible metastatic cancer
- Lambert-Eaton syndrome –> Proximal muscle weakness that improves with recurrent use + autonomic dysfunction (orthostasis, dry mouth, etc.) + Decreased reflexes
- Syringomyelia –> Upper extremity weakness with loss of pain/temperature sensation over upper extremities and back/shoulders in a “cape-like” distribution
38) A 72-year-old woman is brought to the physician because of a 24-hour history of severe right ear pain…
Herpes zoster
- Elderly patient presenting with weakness of entire right face (including forehead) + painful ear rash most concerning for Ramsay-Hunt syndrome (due to varicella zoster [AKA herpes zoster])
- Unable to close eye –> Forehead involvement –> CN7 palsy (rather than motor weakness due to pathology involving motor cortex)
- Common causes of Bell’s palsy:
- HSV (most common!)
- VZV (leads to Ramsay-Hunt syndrome with painful vesicles within ipsilateral ear)
- Sarcoidosis
- Salivary tumors
- Lyme disease (BILATERAL Bell’s palsy)
39) An 18-year-old woman is brought to the emergency department 30 minutes after a 5-minute generalized tonic-clonic…
Folic acid
- Young woman with history of myoclonic jerks presents in a post-ictal state following a generalized tonic-clonic seizure –> She should receive folate supplementation alongside her anticonvulsant given anticonvulsants commonly lead to folate deficiency
- Folate deficiency in young woman –> Neural tube defects in fetus (which is why young women should take folate supplementation, especially when trying to become pregnant)
40) A 22-year-old college student comes to the student health center after an episode during which he found himself unable…
Reassurance
- Young man with increased life stress presents following a single episode of brief paralysis upon waking with otherwise normal history and exam, most consistent with sleep paralysis –> Unless it becomes recurrent, can be managed conservatively with reassurance and education
- Key idea: During REM sleep our muscles are paralyzed such that we don’t act out our dreams, with sleep paralysis occurring when patients transition to wakefulness with a few seconds of residual REM-related sleep paralysis
- Key idea: Narcolepsy is sometimes associated with sleep paralysis, in addition to hallucinations occurring while falling asleep (hypnagogic) and upon waking (hypnopompic)
41) A 6-month-old boy is admitted to the hospital for evaluation of spasms. The child’s father and a paternal aunt…
Tuberous sclerosis
- Newborn with family history of seizures, intellectual disability and angiofibromas (acneiform lesions without comedones) presents with episodes of spasms with evaluation notable for ash-leaf spots and subependymal calcifications on head CT, most concerning for tuberous sclerosis
- Tuberous sclerosis leads to HAMARTOMAS:
- Hamartomas (in CNS and skin)
- Angiofibromas (papules on face without comedones)
- Mitral regurgitation
- Ash-leaf spots (hypopigmented spots)
- Rhabdomyoma (cardiac tumor)
- Tuberous sclerosis
- autosomal dOminant
- Mental retardation
- Angiomyolipoma
- Seizures and Subependymal calcifications
- Shagreen patch
- Neurofibromatosis –> Neurofibromas, cafe au-lait spots, optic glioma, pheochromocytoma, schwannomas
- Sturge-Weber syndrome –> Port-wine stain on face + seizures + glaucoma
42) A 52-year-old man comes to the physician because of progressive bilateral leg pain over the past year. The pain…
Lumbar spinal stenosis
- Middle-aged man with atherosclerotic risk factors presents with bilateral exertional pain in the thighs and calves that improves when bending over with diminished pedal pulses, most concerning for lumbar spinal stenosis
- Test-taking tip: The patient’s risk factors and presentation have features consistent with both spinal stenosis and peripheral artery disease, with the positional aspect of the pain being a very specific finding for spinal stenosis (always try to identify the most unique aspect of the presentation that you need to explain with your answer!)
- Key idea: Both claudication due to peripheral artery disease and pseudoclaudication due to spinal stenosis will present with exertional leg pain, with differentiating factors including:
- Claudication (PAD)
- Cardiac risk factors (diabetes, HTN, smoking, etc.)
- Reduced lower extremity pulses and temperature
- Reduced hair on legs (indicative of decreased perfusion)
- Pain worse in the calves (distal blood supply affected most strongly)
- Pseudoclaudication (spinal stenosis)
- Positional pain (worse with extension, better with flexion)
- Pain affecting the buttocks/thighs
- Claudication (PAD)
43) A 5-year-old girl is brought to the emergency department by her parents because of a 4-hour history of unsteady gait…
CT scan of the head
- Young child with recent URI presents with acute onset of unsteady gait + vomiting + nystagmus most consistent with acute cerebellar ataxia following the infection, but would be prudent to obtain head imaging to rule out posterior fossa mass vs stroke/hemorrhage vs hydrocephalus
- Key idea: In this instance, although a benign condition is most likely, the differential contains possible emergent situations that could benefit from immediate detection and management
44) A previously healthy 13-year-old girl is brought to the emergency department 1 hour after a generalized tonic-clonic seizure…
- Young immigrant patient presents following a generalized tonic-clonic seizure with CT scan demonstrating calcified lesions most concerning for neurocysticercosis –> Disease is transmitted through consumption of undercooked pork, so best screen for families would be stool O&P looking for tapeworm eggs
- Key idea: Neurocysticercosis classically affects individuals from Latin American countries
- RPR –> Syphillis –> Argyll-Robertson pupil, Romberg joints, aortic aneurysm, etc.
- Histoplasma and Cocci –> Pulmonary disease + lymphadenopathy + erythema nodosum, etc. in patients visiting certain areas of the United States
- Toxoplasma –> Ring-enhancing lesion in immunocompromised patient (e.g., HIV)
- Congenital CMV –> Microcephaly + seizures + periVentricular calcifications
45) A 52-year-old woman comes to the physician because of a 2-week history of moderate pain, numbness and…
Mechanical entrapment of the median nerve
- Middle-aged woman with history of hypothyroidism presents with subacute history of intermittent pain, tingling and numbness in the right palmar surface of the thumb and index fingers that is worse at night and reproducible with tapping of wrist (Tinel’s sign), most consistent with Carpal tunnel syndrome (entrapment of median nerve in carpal tunnel at wrist)
- Key idea: Carpal tunnel often worse at night because a lot of people sleep by flexing wrist and tucking hand under their head, putting a lot of pressure on carpal tunnel
- Note: Carpal tunnel also classically improves when shaking out wrists
- Risk factors for carpal tunnel syndrome (often associated with soft tissue enlargement):
- Hypothyroidism (–> myxedema)
- Diabetes
- Pregnancy (due to increased edema)
- Rheumatoid arthritis
- Acromegaly
- End-stage renal disease (due to amyloid deposition)
- Idiopathic (+/- overuse)

46) An otherwise healthy 77-year-old woman comes to the physician because of a 1-month history of severe dizziness…
Positional oculovestibular testing
- Elderly woman presents with chronic history of dizziness and spinning sensation triggered by rapid head movements that last for <1 minute, most consistent with benign paroxysmal positional vertigo (BPPV) –> Diagnose with Dix-Hallpike maneuver and treat with Epley maneuver
- Peripheral vertigo differential:
- Meniere’s disease –> Recurrent episodes lasting 20 minutes to 24 hours with unique features being hearing loss and tinnitus
- BPPV –> Recurrent episodes last several seconds and are triggered by head movement
- Vestibular neuritis –> One episode lasting on the order of days that often follows a viral URI
- Tilt table test –> Orthostatic hypotension
- Holter monitoring –> Cardiac arrhythmias
- Doppler of carotids –> Concern for carotid atherosclerosis (such as amaurosis fugax)
- EEG –> Seizure
47) A 25-year-old farm worker is brought to the emergency department because of the sudden onset of headache, dizziness…
Wearing rubber gloves
- Young farm worker presents with acute onset of headache, dizziness, nausea/vomiting, bradycardia, diaphoresis and pinpoint pupils, concerning for organophosphate poisoning –> Can be exposed transcutaneously, so patients should be decontaminated and providers should be careful about skin-to-skin contact
- Organophosphate poisoning –> Acetylcholinesterase inhibitor –> Increased acetylcholine –> Increased sweating and parasympathetic functions (lacrimation, bradycardia, miosis, vomiting, diarrhea, etc.)
- Key idea: Organophosphate poisoning treated with anti-muscarinics (atropine) and pralidoxime (regenerates acetylcholinesterase)
48) A 67-year-old woman comes to the physician because of a 6-month history of buttock and leg pain. The pain occurs…
Lumbar spinal stenosis
- Elderly woman with history of type 2 diabetes presents with chronic history of exertional buttock/leg pain better when bending forward with normal peripheral pulses most consistent with spinal stenosis
- Key idea: Both claudication due to peripheral artery disease and pseudoclaudication due to spinal stenosis will present with exertional leg pain, with differentiating factors including:
- Claudication (PAD)
- Cardiac risk factors (diabetes, HTN, smoking, etc.)
- Reduced lower extremity pulses and temperature
- Reduced hair on legs (indicative of decreased perfusion)
- Pain worse in the calves (distal blood supply affected most strongly)
- Pseudoclaudication (spinal stenosis)
- Positional pain (worse with extension, better with flexion)
- Pain affecting the buttocks/thighs
- Claudication (PAD)
- Sacroiliac arthritis –> Ankylosing spondylitis –> Inflammatory back pain (worse upon waking and improves with use) + restricted back movement
49) A 67-year-old man with hypertension is brought to the emergency department 30 minutes after a stroke…
Right lateral medulla
- Elderly woman presents with acute onset of Horner syndrome, paralysis of the right palate with “crossed signs” (loss of pain/temp to opposite sides of face versus body) most consistent with right lateral medullary stroke
- Horner syndrome –> Nonspecific finding of all lateral brainstem strokes, ipsilateral
- “Crossed signs” –> Nonspecific finding of all lateral brainstem strokes, loss of facial pain/temp ipsilateral to lesion
- Palate weakness –> CN 10/11 weakness –> Specific for lateral medullary localization
- HIGH-YIELD: Rule of 4’s below can help you develop system for localizing brainstem lesions (recommend Boards & Beyond video)
- Key idea:
- Medial midbrain –> CN3 and CN4 defects
- Medial pons –> Locked-in syndrome
- Lateral pons –> CN7 defect is specific finding
- Medial medulla –> CN12 defect is specific finding
- Lateral medulla –> CN 10/11 defect is specific finding

50) A 37-year-old woman with a 1-year history of HIV infection comes to the physician because of headache and fever…
Mass lesion within the substance of the right frontal cortex with shift to the left of midline structures
- Young woman with poorly controlled HIV presents with acute headache and fever with unilateral UMN weakness (positive Babinski, increased reflexes), concerning for cerebral toxoplasmosis leading to edema with shift of midline structures
- Key idea: If a patient with HIV presents with ring-enhancing lesions in the brain, the two diagnostic considerations are toxoplasmosis versus CNS lymphoma:
- Toxoplasmosis: Multiple lesions responsive to pyrimethamine-sulfadiazine, patients with poorly controlled HIV
- CNS lymphoma: Single-multiple lesions unresponsive to pyrimethamine-sulfadiazine
- Markedly enlarged sulci with loss of brain matter –> Neurodegenerative disease (Alzheimer’s disease, Parkinson’s)
- Markedly enlarged ventricles with minimal changes in sulci –> Normal pressure hydrocephalus –> Wet, wacky, wobbly –> Urinary incontinence, dementia, ataxia
We are not affiliated with the NBME, USMLE or AAMC.
The answer explanations may not be reproduced or distributed, in whole or in part, without written permission of Step Prep.
